
In its early stages, renal cell cancer usually causes no noticeable symptoms. Symptoms may occur only when the cancer grows and begins to press on surrounding tissues or spread to other parts of the body. The symptoms vary considerably from person to person. Some people never develop any symptoms; the cancer is found when they undergo imaging tests, such as a CT scan, for another reason. In a study in the Journal of Urology, approximately 53% of people with localized renal cell carcinoma had no symptoms.
Symptoms of renal cell cancer may include the following:
* Hematuria (blood in the urine)
* Pain in the flank (side or back above the waist) that will not go away
* Noticeable mass (lump) in the flank
* Weight loss
* Fatigue (feeling tired)
* Loss of appetite
* Fevers
* Night sweats
* Malaise (feeling "blah")
* Anemia ("low blood" due to an abnormally low number of red blood cells)
Other symptoms may result from metastatic renal cell cancer in the bones, lungs, or elsewhere. If the disease attacks the bones, for example, it can cause bone pain, which is deep and achy.
Renal cell cancer can also cause a number of conditions called paraneoplastic syndromes. These are problems caused by the tumor when it releases cytokines (chemicals involved with the immune system) or hormones. Cytokines may or may not cause symptoms, and a person may unknowingly have one or more of the following symptoms.
* High blood pressure
* Hypercalcemia (high level of calcium in the blood)
* Polycythemia ("high blood" due to an abnormally high number of red blood cells)
* Liver disorders
* Muscle weakness
* Neuropathy (numbness, tingling, or burning pain in one or more areas)
* Amyloidosis (abnormal protein deposition in the body)
When to Seek Medical Care
Contact a health care provider if any of the following symptoms occur:
* Blood in the urine
* Pain in the side that will not go away
* A lump in the side or belly
* Unexplained fevers
* Weight loss
* Night sweats
If any unexplained symptoms last more than a few days, or if a person just "doesn't feel right," make an appointment with a health care professional.
Do not ignore these symptoms or hope that they will just go away. They may not be cancer, but if they are, an early diagnosis is better. The earlier a cancer is diagnosed and treated, the better the chances are of a full recovery.
Several different types of cancer can develop in the kidney. Conventional or clear cell renal cell cancer, also known as renal cell carcinoma, is by far the most common type of kidney cancer in adults. Renes is the Latin word for kidney. Renal cell carcinoma accounts for about 85% of cancers arising from the kidney. Renal cell carcinoma develops in the tubules of the kidney, part of the filtering system.
Cancer occurs when normal cells undergo a transformation. During this transformation, the cells grow and multiply without normal controls.
* As the cancer cells multiply, they form an area of abnormal cells.
* As the cells continue to multiply, they form a mass called a tumor. (Tumors are not always cancer, but all the information about kidney tumors discussed in this article pertains to cancer.)
* Tumors overwhelm surrounding tissues by invading their space and taking the oxygen and nutrients they need to survive and function.
* Tumors are cancerous only if they are malignant-this means that, because of their uncontrolled growth, the tumors invade tissues of neighboring organs such as the liver, colon, or pancreas.
* Cancer cells may also travel to remote organs via the bloodstream or the lymphatic system (a major part of the immune system consisting of organs and lymph vessels, ducts, and nodes that transport lymph from vessels through the bloodstream).
* This process of invading and spreading to other organs is called metastasis. Renal cell carcinoma is most likely to spread to neighboring lymph nodes, the lungs, the liver, the bones, or the brain.
Each year, about 32,000 people in the United States are diagnosed with renal cell carcinoma. Of these diagnoses, most occur in people aged 50-70 years, but the disease can occur at any age. About twice as many men as women develop this cancer, and it occurs in all races and ethnic groups.
Like almost all cancers, renal cell cancer is most likely to be successfully treated when it is found early.
Renal Cell Cancer Causes
The exact cause of renal cell cancer has not been determined. A number of different factors seem to contribute to renal cell cancer. These factors include the following:
* Cigarette smoking doubles the risk of renal cell cancer and contributes to as many as one third of all cases. The more someone smokes, the greater the risk is of that person developing renal cell cancer.
* Obesity is a risk factor. As body weight increases, so does the risk of developing renal cell cancer. This is especially true in women.
* Occupational exposure to petroleum products, heavy metals, solvents, coke-oven emissions, or asbestos
* Cystic kidney disease associated with chronic (long-term) renal insufficiency
* Cystic changes in the kidney and renal dialysis
* Tuberous sclerosis
* Von Hippel-Lindau (VHL) disease, an inherited disease associated with several cancers
* Hereditary renal cancer
* Associated malignancy such as lymphoma
Exams and Tests
Only 10% of people with renal cell cancer have the classic specific symptoms, such as blood in the urine, or a lump or pain in the side. Other people have only vague, nonspecific symptoms, such as fatigue or just not feeling well. Still others have no symptoms at all. A health care provider will gather many different types of information to make a diagnosis. This process includes ruling out conditions that cause similar symptoms. If urinary symptoms occur, referral to a urologist (a doctor who specializes in diseases of the urinary tract) may be necessary.
The following steps may be taken for a health care provider to make a correct diagnosis:
* Medical interview: A health care provider asks questions about the symptoms and how they started, current and previous medical problems, medications, family medical history, work and travel history, and habits and lifestyle.
* Physical exam: This exam is performed to look for abnormalities that suggest a cause of the symptoms.
* X-rays, a CT scan, and lab tests: These studies are usually performed after the interview and physical exam. If the results suggest that renal cell cancer or another cancer may be present, referral to a surgeon, a radiologist, and/or an oncologist (a doctor who specializes in cancer) may be needed.
* Biopsy: A biopsy involves taking a small sample of the tumor. The sample is usually removed via a large needle inserted into the tumor. The sample is examined by a pathologist (a doctor who specializes in diagnosing diseases in tissues and body fluids). Cancer cells in the biopsy sample confirm the diagnosis of cancer. If the diagnosis of kidney cancer is strongly suspected based on x-ray/CT scan studies, biopsies of the kidney are not always done because of the risk of bleeding. The definitive diagnosis of kidney cancer is made at the time of surgery to remove the kidney (nephrectomy).
* Staging: Another series of imaging studies and lab tests are performed to learn more details about the cancer and whether it has spread to other parts of the body. Careful staging is extremely important for planning treatment and predicting the course of the disease.
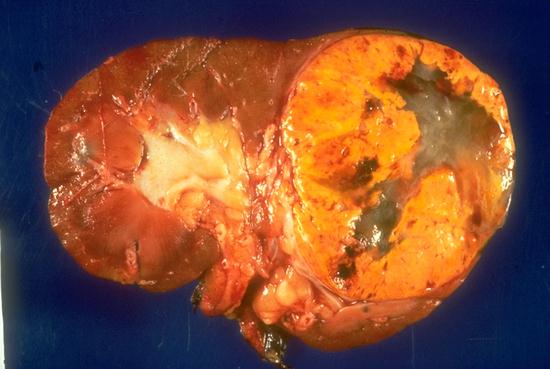
 | Renal Cell Carcinoma Image 1 (Computed Tomography): Large right kidney mass with central necrosis consistent with renal cell carcinoma. There is tumour extension into the right renal vein (arrow). |
Imaging studies
A number of imaging studies are used to evaluate and stage renal masses.
* Intravenous pyelogram (IVP): This study is also called excretory urography. A series of x-rays are taken of the kidneys, ureters, and bladder after a dye is injected into the bloodstream via a vein. The dye allows a much clearer and more detailed image of these organs than a regular x-ray. This study shows less detail than newer scans such as a CT scan and an MRI.
* Arteriography/venography: This study is a series of x-rays of the blood vessels in and around the kidneys after injection of a harmless dye into the bloodstream. Like IVP, this study shows less detail than CT scans and MRIs.
* Ultrasonography: This method uses sound waves (ultrasound) to create an image of the kidneys and surrounding tissues. This safe technique is the same method used to look at a fetus in a mother's womb. This method shows the difference between tumors and other abnormalities such as cysts.
* Computed tomography (CT scan): This study is like an x-ray but shows greater detail than an x-ray and gives a 3-dimensional view of the kidneys and surrounding organs. CT clearly shows the difference between abnormal and normal tissues, and it also shows enlarged lymph nodes.
* Magnetic resonance imaging (MRI): An MRI shows even more detail than a CT scan and shows if areas around the kidneys are affected by the tumor, especially blood vessels.
* Positron emission tomography (PET): This study is recent technology that can show how tissues metabolize sugar. Because cancers take up and metabolize sugar differently than normal tissue, PET imaging can be useful in defining abnormal areas on a CT scan or an MRI.
* Bone scan: A bone scan is recommended for anyone who has bone pain or other symptoms that suggest bone involvement. A chest x-ray or a CT scan can detect cancer spread to the lungs.
Lab tests
The following lab tests are performed to look for paraneoplastic syndromes, to rule out other conditions, and to evaluate a person's overall health before beginning treatment.
* Urine analysis
* Blood tests - Blood cell counts, chemistry, liver and kidney function tests, erythrocyte sedimentation rate, and prothrombin time and activated partial thromboplastin time (clotting studies)
Staging
Staging of renal cell cancer is based on the size of the tumor and the extent of its spread outside the kidney. Like many cancers, renal cell cancer is staged according to the tumor (T), nodes (N), and metastases (M) classification endorsed by the American Joint Committee on Cancer (AJCC). The TNM classification system assigns a T code, an N code, and an M code to each tumor. An X is used if that feature cannot be determined. The combination of these 3 codes determines the disease stage.
* Primary tumor (T) - 0, 1, 2, 3a, 3b, 3c, 4; based on size of tumor and parts of kidney and surrounding area involved
* Regional lymph nodes (N) - 0, 1, 2; based on number of lymph nodes involved
* Distant metastasis (M) - 0 (no metastasis), 1 (metastasis)
AJCC stages
* Stage I - T1N0M0; cancer is 7 cm or smaller in size and confined to the kidney
* Stage II - T2N0M0; cancer is larger than 7 cm and confined to the kidney
* Stage III - T1 or 2, N1M0 or T3a-c, N0-1, M0; cancer of any size that has spread to fatty tissue, blood vessels, or a lymph node near the kidney
* Stage IV - T4; or any T, N2M0; or any T, any N, M1; cancer has spread to multiple lymph nodes; to nearby organs, such as the bowel or pancreas; or to other parts of the body, such as the lung, brain, or bone
Renal Cell Cancer Treatment
The likelihood that renal cell cancer will be cured depends on its stage when it is diagnosed and treated. Renal cell cancers found in the early stages are cured over half the time. Unfortunately, this cancer often is not found until it has reached an advanced stage. The chance of curing metastatic (stage IV) renal cell cancer is small.
Medical Treatment
Treatment of renal cell cancer depends on the stage of the disease and the person's overall health, which determines how well that person is able to tolerate various therapies. A medical team will devise a treatment plan that is tailored specifically for the individual. Therapies that are used for renal cell cancer include surgery, chemotherapy, biological therapy, hormone therapy, and radiation therapy. Clinical trials (tests of new medicines) may be appropriate for some patients with kidney cancer. A person may undergo a single therapy or a combination of therapies.
Generally, surgery is the best treatment for renal cell cancer that has not metastasized. For more information, see Surgery.
Chemotherapy is the use of strong drugs to kill cancer cells.
* Unfortunately, chemotherapy has less benefit in renal cell cancer than other cancer diagnoses.
* Chemotherapy shrinks the tumor in some patients with kidney cancer, but this period of remission does not usually last long.
* Chemotherapy drugs may be given singly or in combinations.
* Chemotherapy typically has side effects such as nausea and vomiting, weight loss, and hair loss. Chemotherapy can also suppress production of new blood cells, leading to fatigue, anemia, easy bruising or bleeding, and increased risk of infection.
Hormone therapy involves taking a hormone to kill cancer cells. Several different hormone preparations have been tried in renal cell cancer in the past, but these agents are less effective than chemotherapy and are no longer used frequently.
Biological therapy, sometimes called immunotherapy, tries to boost the body's own immune system to fight and kill the cancer, by using substances made naturally by the body. These substances are copied in a laboratory and injected into the body.
* Biological therapy is often reserved for metastatic renal cell cancers that cannot be cured by surgery.
* The most successful immunotherapy drugs in metastatic renal cell cancers are interleukin-2 (IL-2) and interferon alfa (IFNa).
* These agents have side effects that can be very severe, including high fevers and chills, dangerously low blood pressure, fluid around the lungs, kidney damage, intestinal bleeding, and heart attacks. Despite these problems, selected patients can tolerate these treatments and can achieve prolonged remissions. For instance, some patients are alive 15 years or longer after having received high-dose IL-2 for metastatic kidney cancer.
* Because lower doses of medications cause fewer and less severe side effects, low doses of these agents are being tested in combination with each other, with other cytokines and immune cells, and with chemotherapy drugs.
* Many areas of research are active in kidney cancer treatment, including investigation of agents that block blood vessel formation (necessary for growth of the kidney cancer), drugs that block division of kidney cancer cells, vaccines, and new drugs that boost the immune system.
Radiation therapy uses a high-energy radiation beam to kill cancer cells. Renal cell cancers typically are resistant to radiation. Some people undergo radiation therapy after surgery to kill tumor cells that remain. Radiation therapy is often used to relieve symptoms in persons with metastatic disease or who cannot undergo surgery because of other medical conditions.
Because metastatic renal cell cancer is largely incurable with currently available forms of systemic therapy, patients with metastatic renal cell cancer are encouraged to discuss innovative clinical trials with their physicians before making a final decision.
Medications
The goals of drug therapy are to induce remission, to reduce symptoms, and to prevent complications.
Anticancer agents: Chemotherapy often has little affect in renal cell cancer. However, in a small minority of people, chemotherapy can relieve symptoms and sometimes delay growth of the cancer. The best chemotherapy drugs for renal cell cancer are as follows:
* Vinblastine (Velban, Alkaban-AQ)
* Gemcitabine (Gemzar)
* 5-fluorouracil (Adrucil)
Hormones: Hormone therapy shrinks renal cell cancer in fewer than 5% of cases. Medroxyprogesterone (Provera) is an example of a hormone used to treat renal cell cancer.
Biological agents: These agents are most often used in people with metastatic renal cell cancer.
* Interleukin-2 - Known by the biological name of aldesleukin (Proleukin)
* Interferon alfa-2a (Roferon A) and interferon alfa-2b (Intron A)
* Bevacizumab (Avastin) - Recently approved for colon cancer but is investigational at this time for renal cancer
Surgery
Removal of the diseased kidney (nephrectomy) is the standard treatment of renal cell carcinoma. People can live normally with one kidney if that kidney is healthy. The 3 main types of nephrectomy are as follows:
* Partial nephrectomy: The tumor and part of the kidney around the tumor are removed. The partial nephrectomy is performed mainly in people who have problems with their other kidney. This treatment is being investigated by surgeons to determine if it is as effective as the standard procedures to remove the kidney, as described below.
* Simple nephrectomy: The cancerous kidney is removed.
* Radical nephrectomy: The cancerous kidney, adrenal gland, and surrounding tissue are removed.
Nephrectomy may be performed with a large incision or via laparoscopy. Laparoscopy is a technique that removes the kidney through a very small incision. Laparoscopy leaves a smaller scar and requires less time in the hospital. It is used for people with small kidney cancers.
Nephrectomy may cure the disease if it has not spread to other parts of the body. Sometimes people with metastatic disease undergo a nephrectomy to relieve symptoms such as bleeding, pain, high blood pressure, high levels of calcium in the blood. Nephrectomy alone cannot cure metastatic renal cell carcinoma, but recent studies suggest that selected patients who receive immunotherapy after a nephrectomy for metastatic disease have a longer survival rate than those who do not undergo nephrectomy. In some cases, a solitary metastatic tumor can be removed, increasing chances of remission.
Another procedure called arterial embolization (plugging up the artery) is sometimes used for people who cannot undergo surgery. Different methods have been used to embolize kidneys, including injection of small pieces of a special gelatin sponge, plastic microspheres, ethanol, or chemotherapy. The injected agent can block the artery and prevent blood from getting through to the kidney and the tumor. The tumor cannot live without blood, and it dies.
Follow-up
After treatment is completed, a urologist/oncologist will perform regular evaluations, typically every 4 or 6 months for as long as 5 years. These visits include history and physical examination along with imaging studies, such as chest x-rays and abdominal CT scans, to monitor the condition and lab tests to make sure the kidneys and other organs are working properly.
Prevention
The best way to avoid renal cell cancer, and many other cancers, is not to smoke. Eating a healthy, balanced diet and maintaining a healthy weight also reduce the risk of cancer.
Outlook
The outlook for a person with renal cell cancer depends on the stage, the type of treatment received, the complications of the disease, and the person's overall condition. In general, the lower the stage at the time of treatment, the better the prognosis. Tumors confined to the kidney have the best chance of cure. About 25-30% of people have metastatic disease at diagnosis.
In people whose disease is limited to the kidney area, 20-30% develop metastatic disease after nephrectomy. Those who have a long disease-free interval between nephrectomy and the appearance of metastases usually do best. Those with a solitary metastasis to a lung usually have the best outlook, since such metastases can often be treated by surgery. Patients with more extensive metastatic disease may benefit from biological therapy and should see an oncologist who specializes in these treatments.
Support Groups and Counseling
Living with cancer presents many new challenges, both for the people with cancer and for their family and friends.
* People with cancer probably have many worries about how the cancer will affect them and their ability to "live a normal life," to care for their family and home, to hold their job, and to continue the friendships and activities they enjoy.
* Many people feel anxious and depressed. Some people feel angry and resentful; others feel helpless and defeated.
For most people with cancer, talking about their feelings and concerns helps.
* Friends and family members can be very supportive. They may be hesitant to offer support until they see how someone is coping. If people with cancer want to talk about their concerns, they should let someone know.
* Some people do not want to "burden" their loved ones, or prefer talking about their concerns with a more neutral professional. A social worker, a counselor, or a member of the clergy can be helpful if they want to discuss their feelings and concerns about having cancer. A surgeon or an oncologist should be able to recommend someone.
* Many people with cancer are helped profoundly by talking to other people who have cancer. Sharing concerns with others who have been through the same thing can be remarkably reassuring. Support groups of people with cancer may be available through the medical center where treatment was received. The American Cancer Society also has information about support groups all over the United States.
For more information about support groups, contact these agencies:
* American Cancer Society - (800) ACS-2345
* Kidney Cancer Association - (800) 850-9132
American Cancer Society
(800) ACS-2345
Cancer Information Service, National Cancer Institute, National Institutes of Health
(800) 4CANCER
(800) 422-6237
Kidney Cancer Association
1234 Sherman Avenue, Suite 203
Evanston, IL 60202-1375
(800) 850-9132

No comments:
Post a Comment