The case for prophylactic fever treatment (every year).
The case for prophylactic fever treatment (every year). Fever is one of the pathophysiological symptoms accompanying the response of the host to infection and inflammation.
Although the adaptive value of the fever response has been well documented in laboratory studies, its role in clinical
medicine is still under debate.
Two of the hypotheses studied state that endogenous mediators of fever may be involved
in establishing the Th1 immunologic phenotype of the host and in improving general immunologic surveillance.
It is known that these factors play a significant role in defence against tumour cells. Therefore, in the present study
we tested the hypothesis that patients diagnosed with cancer reveal a history of fewer fevers during the disease
than control, healthy volunteers.
18 questions were asked concerning the history of fever prior to diagnosis from
355 persons suffering from cancer, and 244 healthy controls, matched for age and living in Poland. Cancer patients
reported a lower incidence of fever during illness than controls. The percentage of cancer patients and controls
who reported no fever during infections was 83.10% and 56.97%, respectively.
Similarly, 16.90% of cancer patients
and 43.03% of controls reported always experiencing fever during infections. The results of our study support the
hypothesis that during their lifetime cancer patients experience less fever during infection than healthy controls.
Key words: fever, infection, cancer, allergy, spontaneous regression
INTRODUCTION
Fever is a specific and well-coordinated pathophysiological
phenomenon associated with infections and trauma, and
manifested by an increase of body core temperature above
normal. It is a part of an acute phase response (APR) - an early
inflammatory response consisting of a host of immunologic,
endocrinologic and neurologic alterations. APR results in
metabolic and behavioural changes collectively called 'sickness
behaviour' [1, 2]. Thus, fever has a significant diagnostic
value which, however, is mostly regarded as an unpleasant
and preventable weakening phase of disorder. In spite of the
overwhelming antipyretic therapy and widespread use of the
fever-preventing drugs, there is ample evidence demonstrating
that fever correlates with increased survival and better
prognosis during microbial infections [3, 4, 5].
Studies into the mechanism and phylogeny of fever indicate
that fever evolved as a constituent of the innate immune
response [4, 6]. Thus, from the biological point of view, fever
is an adaptive response in interactions between the host
and the pathogenic microorganisms. The key steps of the
mechanism of fever have been thoroughly investigated during
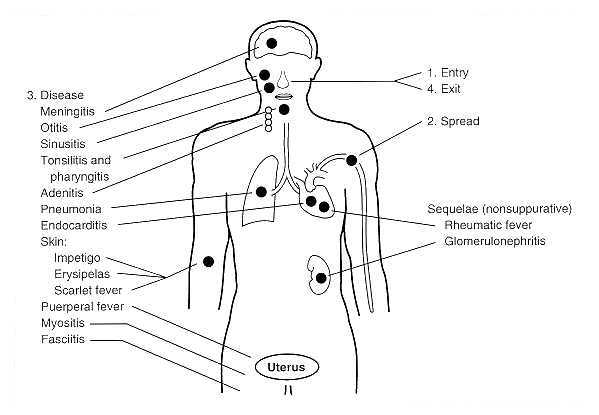
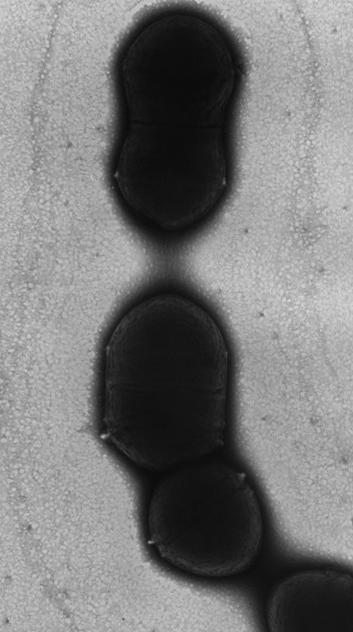
the last decades. Briefly, fever is triggered by microbial factors
and products known as 'exogenous pyrogens' or 'pathogen
associated molecular patterns' (PAMPs). Structures such as
lipopolysaccharides (LPS), peptidoglycans, porin complexes,
lipoteichoic acid, lipoarabinomannans, bacterial DNA,
mycoplasma lipoproteins, staphylococcal and streptococcal
proteinaceous superantigens constitute a major group of the
pyrogens of gram-negative, gram-positive and mycobacterial
origin [7-12]. In response to the PAMPs, the immune cells
of an infected organism generate a host of mediators called
'endogenous pyrogens'. Among them are cytokines such as
IL-1, IL-6 and TNF-á [14]. Endogenous pyrogens stimulate
the production of prostaglandins of the E series (PGE2) which,
in turn, act on the fever-mediating thermoregulatory region
of the preoptic area of the anterior hypothalamus to shift
upward a thermoregulatory set-point. The presented scheme of
molecular events leads to the stimulation of thermoregulatory
effectors to gain body heat and to drive body core temperature.
Although the net benefit of elevated temperature is still under
debate, it has been demonstrated that fever stimulates number
of key mechanisms of the defence against infections; among
others, it stimulates T cells proliferation and differentiation,
B cells proliferation and the production of antibodies, secretion
of interferons, phagocytosis, and the migration of macrophages
and neutrophils [15, 16, 5].
Despite the well documented ubiquity of fever, there are
clinical reports suggesting a decreased frequency of fever, or
even the lack of capability of generating fever within certain
groups of patients. Fewer fevers have long been recognized,
especially amongst cancer patients. As early as 1855, the
English surgeon John Laurence acknowledged the fact that
cancer patients have a "remarkable disease-free history" [17].
Since then, clinical oncologists have often reported that in
their history cancer patients stressed that they were almost
never ill, and had never been feverish before the onset of
cancer. Consequently, it has been postulated that a prolonged
lack of fever can be considered as a threat of cancer [18]. Also,
the more recent studies of Witzel (1970), Newhouse et al.
(1977), Remy et al. (1983), Grufferman et al. (1982), Ronne
(1985), Van Stensel-Moll et al. (1986), Grossarth-Maticek et
al. (1987), Abel et al. (1991), and Kolmel et al. (1992) [19-27],
among others, have supported the conclusion that deficiency
of fever in the medical history of the patient corresponds
with high risk of cancer. In the present paper we also report a
lower frequency of fever in the population of tumour patients
compared to healthy volunteers.
MATERIALS AND METHODS
The study was conducted during a relatively short period,
from January 2005 - June 2006. Retrospective information
on fever and fever disorders was obtained from 355 cancer
patients and 244 healthy volunteers by use of a questionnaire.
To collect the information we cooperated with the following
health care institutions: The Polish Amazons Club, The
House of Social Assistance in Toruñ, and the Academy for
Fighting with Cancer and Public Hospital in Inowroclaw.
Each patient had a documented tissue diagnosis of cancer
from pathology records. The majority of the examined patients
were from the Kujawsko-Pomorskie province, and the healthy
control volunteers were randomly selected from the same
area. The respondent cohort consisted of 350 women and
249 men. The average age was 52 (ranging from 16-96 years
old) and 57 (ranging from 17-95 years old) for women and
men, respectively. All participants signed the consent for
taking part in the questionnaire studies. Only completely
fi lled in questionnaire forms were analyzed. The collected
forms were entered into the Access Database for evaluation and
statistical analyses. The chi-square test was used to compare
rates of occurrence between patients with cancer and healthy
people.
RESULTS AND DISCUSSION
Nowadays, it is well documented that fever directly activates
defence against various dangers (including cancer cells) [28,
29]. It is also well known that various microbial stimuli are
necessary for the normal maturation of the immune system
[30]. This discovery places in an unfavourable light the
situation of cancer patients, who very often stress that before
diagnosis they could be considerate as examples of health.
They had never been ill, and even if they had, they almost
never been feverish. Moreover, the observation that cancer
patients who experienced a feverish period after surgery
survived significantly longer than patients without fever,
and the fact that spontaneous tumour remission was observed
mostly after a fever, confirms the significant meaning of this
mechanism for a patient's recovery [31]. For this reason we
performed an epidemiological study. Our aim was to discover
whether there is a difference in the frequency of fever episodes
between healthy people and cancer patients, and to check
peoples' attitude to fever. We compared 355 forms fi lled out
by cancer patients, with another 244 forms from healthy
people (Table 1).
It was observed that the frequency of feverish events during a
whole life significantly differed between the 2 groups: 83.1% of
cancer patients, compared to 56.97% of control group, declared
that they never or almost never have been feverish (Table 1,
Fig. 1). Among the cancer patients only 16.9% did recall of
getting fever in compare to 43.03% of control people. This
data are in accordance with Engel's results, who compared 300
cancer patients with 300 patients not suffering from cancer.
People who had never experienced febrile infectious disease
were 46 times more likely to have developed cancer than those
who had had febrile infections [32]. More recent studies also
confirm these earlier results. In 1987, Grossarth-Maticek et.
al., after questioning 1,353 people, indicated that: "episodes
of high fever during the entire life span in the case of an acute
illness as a typical reaction are inversely related to later cancer
incidence" [25]. In 1991, Abel et al., in a case-control study
with 255 cancer patients compared with 230 controls, showed
that patients who had the highest risk for cancer were those
with a low "infectious index" [33]. Kolmel demonstrated the
essential meaning of the number of febrile illnesses, their
length and level concerning the risk of melanoma incidence.
The undergoing of a minimum of 3 fevers above 38.5 °C
decreased the risk of melanoma incidence by approximately
40% [34].
The surprising result of our research was that above 56% of
healthy volunteers have never been feverish (Fig. 1). During 17
months of our research we found a few cases from the control
group who were subsequently diagnosed as cancer patients.
It is possible that such cases were or will be more frequent.
This could be the cause of erasing the difference between two
groups of our responders.
We observed that there were no significant differences
between cancer patients and healthy control volunteers in
the highest temperature value they recalled having during
their lives. The average, highest temperature during whole life
for the control group was 39.5 C ± 0.8, and for cancer patients
39.2 C ± 0.9. We conclude that this part of cancer patients
who had been feverish (16.9% of cancer patients) can develop
the same level of fever as healthy people. This suggests that
carcinogenesis of some cancers may be indirectly connected
with inefficient generation of fever.
There exist epidemiological studies supporting the
hypothesis that there is an association between febrile
infectious childhood diseases and subsequent cancer risk.
Kolmel et al. demonstrated an inverse relation between the
number of children's febrile infections and the incidence of
malignant melanoma in 271 controls versus 139 melanoma
patients [27]. Exposures to such infections were also associated
with a reduced risk for ovarian cancer [35, 20] and multiple
cancers combined [33, 36]. We investigated whether the
assertion that children's contagious illnesses have a preventive
eff ect on cancer is true or not. After our respondent cohort
examination, significant differences were observed in the
incidences of children's contagious illnesses such as: mumps,
rubella and chicken pox (Tab. 2, Fig.3).
The study by Hoff man et al. suggests that chickenpox and
mumps were associated with an increased risk of cancer [37].
We demonstrate that healthy volunteers suffered from such
disease more often than cancer patients. Our results are in
accordance with Newhouse data who found lower incidence
of mumps, measles and rubella in the cancer group [20].
Hoffman et al. suggested that no significant reduced risk
is seen between cancer and rubella [37], whereas our data
and data by Newhouse showed a lower frequency of rubella
for cancer patients, compared to healthy people. Only data
concerning measles are in accordance - we did not observe any
statistically significant difference in the mortality between
cancer patients and healthy people. We conclude that because
of divergent results, no final statement on the association
between childhood disease and cancer may be made. However,
taking into consideration our results and published data we
must stress that febrile contagious illnesses during early life
are probably not sufficient to protect against cancer because
many of our cancer patients had suffered from such diseases.
We can therefore suppose that not only infection is important
for the stimulation of the immune system against cancer.
We would like to emphasize that infection connected with
fever, which occurs directly before or at the beginning of cell
transformation, is probably of the greatest significance. Our
stance is in accordance with results of Kolmel et al. who also
stressed that febrile infectious childhood diseases were less
protective against cancer than adult febrile infections [27].
It is known that endogenous mediators of fever play a
significant role in defence against tumour cells [38, 39]. We
hypothesize that these factors may be involved in establishing
the Th1 immunologic phenotype of the host. We suppose
that cancer patients who had never been feverish, prefer Th2
phenotype. Similarly, allergy is an immunological disorder
with a predominant Th2 inflammatory response [40]. The
debate about the relationship between allergy and cancer is
not recent [41]. The "hygiene hypothesis" proposes that lack
of early life infections may up-regulate allergic disorders [42].
We found an appreciable difference in the incidence of allergy
between cancer patients and healthy volunteers (Table 1,
Fig. 4). If a decrease in the number of infections is essential
for allergic disorders and for cancer, it is surprising that only
5.92% of cancer patients, compared to 22.13% of the control
group, suffered from allergy. Moreover we have data which
suggest that cancer and allergy exclude one another (data not
published). The question whether allergy really is a protective
factor for cancer, remains unanswered. However, efficient
redirecting the Th2 response in favour of Th1 will probably
be most essential for both disorders.
The second part of our questionnaire form contained
questions to check people's general attitude to fever (Table 1).
We discovered that people regard the 2 notions -- fever and
illness -- as being identical. A small rise of temperature
from 36.6 °C to 37.5 °C by both groups was treated as an
uncomfortable symptom (Table 1, Fig. 5). The temperature
regarded as fever by cancer patients was 37.82 °C ± 0.4; by
control 37.83 °C± 0.5. People tried to eliminate this disparate
state, in spite of the fact that it is a symptom which informs the
body of the danger related to infections. As mentioned earlier,
on the one hand fever may directly debilitate the pathogen, on
the other hand it induces a cascade of host defence mechanism
that increases the action of the immune system [15, 16].
The rise in body temperature is closely related to the ability
to increase cyclooxygenase (Cox) products of arachidonic
acid (especially prostaglandin PGE2). There are actually 2
Cox enzymes -- Cox-1 and Cox-2 -- both of which produce
prostaglandins that promote inflammation, pain, and fever.
Nonsteroidal anti-inflammatory drugs (NSAIDs) block the
Cox enzymes and reduce prostaglandins throughout the
body. In consequence, ongoing inflammation, pain, and
fever are reduced [43]. Because of easy access, nonsteroidal
anti-inflammatory drugs are very popular. Nowadays almost
everybody can reduce or block fever. The necessity for using
medicines against fever because of the rise in body temperature
was declared by 91.4% of people in the control group, and
87.8% of the cancer patients (Fig. 6). We found that 67.96%
of the control group and 74.6% of cancer patients take these
medications before their temperature reaches 38 °C (Table 1).
Moreover, 60.89% of the control group and 51.42% of cancer
patients take medicines against fever always, or almost always,
even after a small rise in body temperature (Fig. 7). For this
reason we can suppose that episodes of really high and long-
lasting fever actually do not happen. There are a number of
prospective and retrospective studies indicating that febrile
infections lower the risk of cancer, and can be associated
with the spontaneous remission of various tumours [44, 28].
Early use of NSAIDs may deprive us of this chance. In 1998,
Mastrangelo et al. revealed that a reduction of infections in
the second half of 20th century caused an increase in cancer
cases. They discovered that a 2% decrease of febrile illnesses
in one year correlated with a 2% increase in tumors after
10 years [45]. This reduction of infections is undoubtedly
connected with so-called "increase in life hygiene" and with
the use of NSAIDs and antibiotics. Taking into consideration
the influence of fever on the immune system, we consider that
the use of NSAIDs should be more prudent.
Fever is a very important mechanism that supports our
immunological system. Some disorders (cancer, allergy)
seem to be preceded by a lack of fever. Our study confirmed
this notion, despite the fact that it was performed during a
relative short period (17 months). Whether this lack of fever
starts before carcinogenesis or is a consequence of a longterm
process which leads to cell transformation, remains
unresolved. Moreover, we found that more than 72% of all
respondents had never been feverish. It is an open question
whether or not the rare fever episodes evolved naturally, or
are the results of frequent switching off of this mechanism
using NSAIDs which, as we established, people often take
unquestioningly. It is possible that with the passing of time
the immune system ceases developing fever at all and we would
be totally dependent on medicine.
The increase of life hygiene and using NSAIDs is also
connected with the high incidence of allergy. In our study,
we discovered that only small part of cancer patients who
had never been ill and had never been feverish, suffer from
allergy, even though some data suggest that infections are
very essential for protection against cancer, as well as allergy.
This problem should be meticulously examined. It is possible
that artificial induction of fever will be helpful in therapies
against both disorders, and research on this subject haa already
been started [46, 47]. However, nowadays we do not have an
answer to the question: which part of the mechanism of fever
is involved in decreasing risk of cancer and allergy, and which
part participates in the induction of tumour prevention and
remission.
FULL TEXT WITH GRAPHICS
by S Wrotek -
2009http://www.jpccr.eu/archive_pdf/2009_vol_3_nr_1/jpccr_05_str_31_35_Wrotek_et_al.pdf ... sauna drives up the body temperature. It is actually a prophylactic fever ...

(the world's ugliest cat)
Biological basis of the behavior of sick animals
References and further reading may be available for this article. To view references and further reading you must
purchase this article.
Benjamin L. Hart
Department of Physiological Sciences, School of Veterinary Medicine University of California, Davis, CA 95616, USA
Received 1 February 1988.
Available online 18 October 2005.
The most commonly recognized behavioral patterns of animals and people at the onset of febrile infectious diseases are lethargy, depression, anorexia, and reduction in grooming. Findings from recent lines of research are reviewed to formulate the perspective that the behavior of sick animals and people is not a maladaptive response or the effect of debilitation, but rather an organized, evolved behavioral strategy to facilitate the role of fever in combating viral and bacterial infections. The sick individual is viewed as being at a life or death juncture and its behavior is an all-out effort to overcome the disease.
Finally the notion of a
prophylactic fever foranimals such as
...... A modest
prophylactic fever during the activeperiod may have some
...